Acute renal failure may be caused directly by kidney disease or by external abnormalities that affect kidney function, such as:
- Shock due to decreased blood volume, leading to reduced blood flow to the kidneys, such as from bleeding, dehydration, or acute pancreatitis.
- Heart and vascular diseases that reduce blood supply to the kidneys, such as myocardial infarction, heart failure, and severe hypertension.
- Severe infections, such as malaria, leptospirosis, and septicemia.
- Kidney diseases, such as acute glomerulonephritis and acute pyelonephritis.
- Vascular abnormalities in the kidneys, such as renal artery stenosis and renal embolism.
- Obstructions in the urinary tract, such as urinary stones, renal ligation due to complications from abdominal surgery, enlarged prostate, urethral stricture, bladder tumors, cervical cancer, etc.
- Snake bites, such as from a Russell's viper or sea snake.
- Wasp stings, bee stings.
- Side effects from medications or chemicals, such as non-steroidal anti-inflammatory drugs, ACE inhibitors, sulfonamides, kanamycin, gentamicin, amikacin, cyclosporine, amphotericin B, iodine contrast used in special X-ray examinations, etc.
- Complications from pregnancy, such as preeclampsia and premature placental abruption.
- Others, such as hemolysis and liver failure.
Chronic renal failure is most often caused by complications from diabetes and untreated hypertension.
It may also result from chronic kidney diseases such as chronic glomerulonephritis, chronic pyelonephritis, nephrotic syndrome, kidney stones, and polycystic kidney disease*.
Additionally, it can be caused by conditions such as gout, systemic lupus erythematosus (SLE), high uric acid levels, high calcium levels, AIDS, medication toxicity (such as painkillers, antipyretics like phenacetin, non-steroidal anti-inflammatory drugs, lithium, cyclosporine, cancer medications, etc.), and toxicity from substances like lead or cadmium.
For acute renal failure, a prominent symptom is producing less than 400 ml of urine in 24 hours or no urine output at all (no sensation of needing to urinate, and catheterization does not increase output). Soon after, the patient may experience fatigue, loss of appetite, nausea, and vomiting. If left untreated, the patient will eventually become lethargic, confused, suffer seizures, and lose consciousness.
Patients may have a history of medication use or pre-existing illnesses such as fever, high blood pressure, heart disease, kidney disease, liver disease, snake bites, insect stings, bleeding, or shock from various causes.
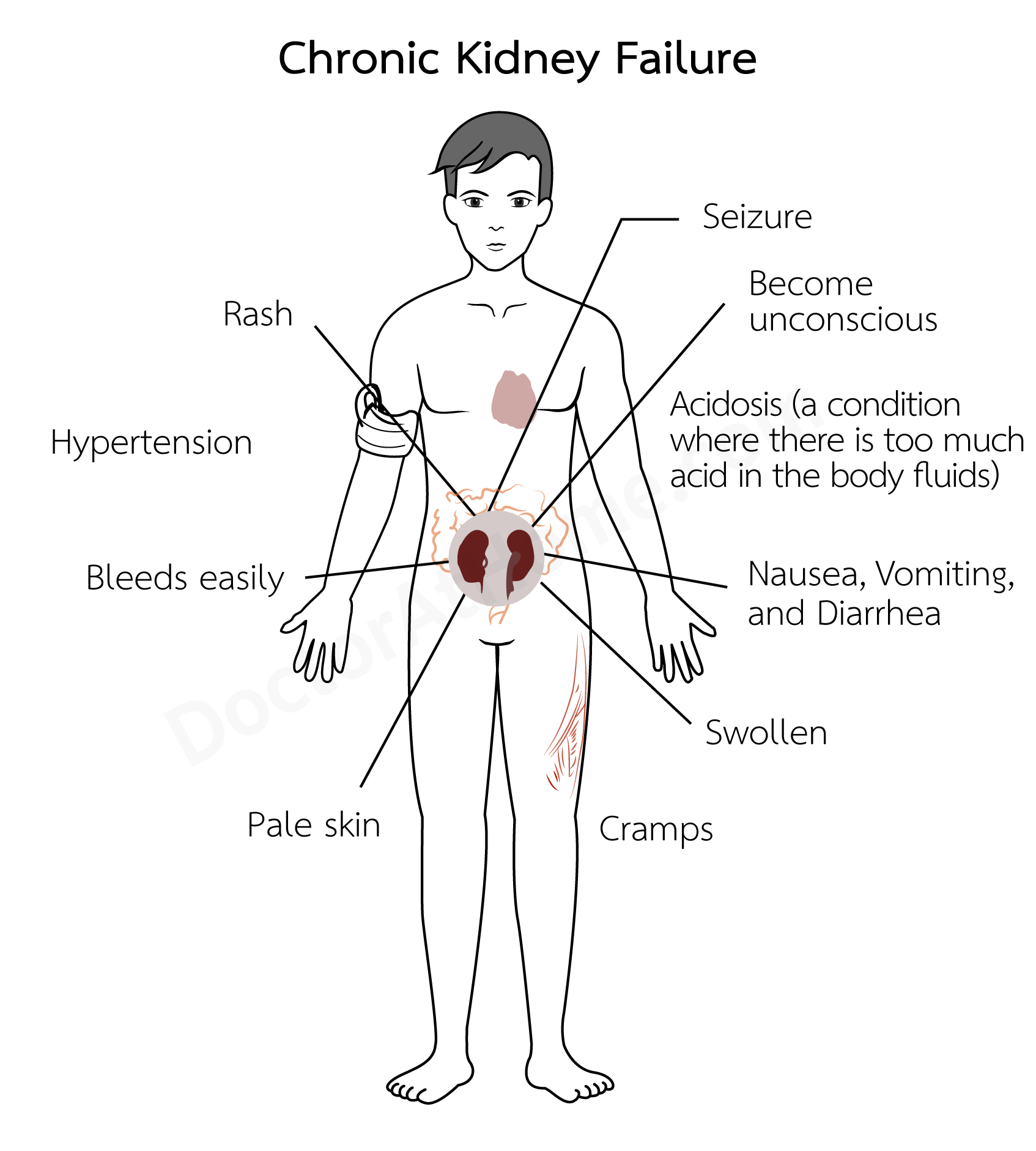
In chronic renal failure, symptoms depend on the severity of the disease. Initially, symptoms may not be noticeable and are often detected through blood tests (showing elevated creatinine and BUN levels) during health check-ups or when visiting a doctor for other illnesses.
Patients will show clear symptoms when both kidneys are damaged to the point where they function at less than 5% of normal capacity. This is observed through increased and frequent urination, especially at night. Patients may experience fatigue, easy tiredness, loss of appetite, nausea, frequent diarrhea, insomnia, headaches, lack of concentration, blurred vision, dry and darkened skin, itching, and numbness in the hands and feet.
Some may also experience shortness of breath, hiccups, muscle cramps, palpitations, chest pain, swelling, or bleeding under the skin as small red or greenish spots, or vomiting or passing blood in stools.
In end-stage disease, patients may become lethargic, experience seizures, and lose consciousness.
For acute renal failure, due to the kidneys' inability to excrete water, fluid overload occurs in the bloodstream (hypervolemia), leading to high blood pressure and heart failure.
Additionally, high potassium levels in the blood (due to reduced excretion by the kidneys) can cause irregular heartbeat or cardiac arrest. Acidosis (due to reduced acid excretion from protein metabolism) may cause deep, labored breathing. Neurological complications, such as lethargy and seizures, arise from uremia. Easy bleeding due to platelet dysfunction can lead to spontaneous bleeding, vomiting blood, or bloody stools. Pericarditis can develop from the accumulation of BUN (BUN levels above 100 mg/dL), presenting symptoms like fever and chest pain. A weakened immune system makes infections more likely, potentially leading to septicemia.
These complications are severe and can be life-threatening. Additionally, less severe complications may occur, including anemia, due to the kidneys' inability to produce erythropoietin, which is essential for red blood cell production. When it is lacking, red blood cells are not produced properly. High phosphate levels, low calcium levels (causing hand cramps and muscle cramps), high magnesium levels, and high uric acid levels are also possible.
In chronic renal failure, in addition to the complications found in acute renal failure, one might encounter pneumonia, pleuritis, peripheral neuropathy (numbness in the hands and feet), gastritis, high triglycerides, hyperparathyroidism (overactive parathyroid glands), osteomalacia (softening of the bones), reduced testicular function, erectile dysfunction in men, and menstrual irregularities or amenorrhea in women.
Medical diagnosis is initially made based on symptoms, medical history, and physical examination.
In acute renal failure, nothing specific may be found other than symptoms related to the underlying cause (e.g., low blood pressure and rapid pulse in patients with shock, jaundice in liver disease patients, fever in patients with malaria or other infections).
Some may show symptoms like anemia, deep labored breathing, high blood pressure, hand cramps, or muscle cramps. Lung examination with a stethoscope may reveal crepitation.
In later stages, symptoms may include lethargy, seizures, and loss of consciousness.
Chronic renal failure will show detectable signs only in the more advanced stages, such as anemia, high blood pressure, dry and darkened skin, and petechiae and purpura/ecchymosis (small red or greenish spots on the skin).
Some may also exhibit swollen feet (pitting edema), irregular heartbeat, or crepitation heard during lung examination with a stethoscope.
To confirm the diagnosis, doctors will conduct blood tests (showing elevated BUN and creatinine levels, with higher levels indicating more severe disease; high levels of potassium, phosphate, and magnesium; low calcium; acidotic blood; low hemoglobin), urine tests (detecting proteins, glucose, red and white blood cells), X-rays, ultrasound, and other specialized tests. In some cases, a renal biopsy may be performed to examine kidney tissue.
The doctor will provide the following treatment:
1. Acute renal failure: Patients are admitted to the hospital where treatment focuses on the underlying cause and correcting any abnormalities that occur. This includes limiting intake of fluids, sodium, potassium, magnesium, and protein. Diuretics such as furosemide are administered to help expel urine. Sodium bicarbonate may be given to correct blood acidosis, and blood transfusions are provided if there is significant blood loss.
If necessary, dialysis may be needed to remove waste products from the blood.
The outcome of treatment depends on the underlying cause. If the renal failure is caused by a urinary tract obstruction, shock due to decreased blood volume, infections, or toxicity from certain medications, there might be a possibility of complete recovery. However, acute renal failure typically develops suddenly and can lead to severe complications, making it potentially life-threatening.
2. Chronic renal failure: If the cause is clear, treat the underlying disease (e.g., medications to control diabetes, high blood pressure, gout, surgical removal of kidney stones, etc.).
Additionally, various abnormalities resulting from renal failure must be managed, such as:
- Restrict protein intake to no more than 40 grams per day (one egg contains 6-8 grams of protein, one cup of fresh milk contains 8 grams of protein, and 100 grams of meat contains about 23 grams of protein).
- Restrict fluid intake calculated from the daily urine output plus other fluid losses (approximately 800 ml/day). For example, if a patient urinates 600 ml/day, the total fluid intake should be 600 ml + 800 ml = 1,400 ml/day.
- Restrict sodium intake, especially if there is swelling or urine output is less than 800 ml/day. Avoid salty foods and seasonings (like fish sauce, soy sauce, and all types of sauces), MSG, preservatives, baking powder, canned food, chili paste, shrimp paste, fermented fish, and pickled foods.
- Restrict potassium intake if urine output is less than 800 ml/day. Avoid high-potassium foods such as dried fruits, oranges, papaya, tamarind, tomatoes, coconut water, beans, stink beans, fried potatoes, shellfish, and animal organs
- Limit magnesium intake by avoiding antacids containing magnesium hydroxide.
- If blood phosphate levels are high or there is acidosis, take calcium carbonate tablets (650 mg) 1 tablet 3 times a day.
- If there is edema, give furosemide diuretics.
- If there is high blood pressure or heart failure, give medications to treat these conditions.
- If there is anemia, blood transfusions may be necessary. In some cases, the doctor may order erythropoietin injections to stimulate red blood cell production (this medication is expensive and can increase blood pressure).
For patients with end-stage chronic kidney disease (typically with blood creatinine and BUN levels exceeding 10 and 100 mg/dL, respectively), medication is not effective. Dialysis is required, which has several methods, including:
- Continuous Ambulatory Peritoneal Dialysis (CAPD): This method can be trained by the doctor for the patient to do at home. It is convenient, but the patient must change the dialysis bag 4 times a day, every day. The doctor will schedule to change the dialysis tubing every 1 month. Patients can work and carry out their duties like normal people.
- Hemodialysis: Often referred to as using an artificial kidney machine. Patients must go to the hospital twice a week.
Both methods can significantly enhance the quality of life, allowing patients to work, exercise, and maintain normal sexual relationships. With these treatments, some patients can live for more than ten years, though costs are relatively high.
For some end-stage chronic renal failure patients, doctors might consider renal transplantation, which is currently the most effective treatment. A successful kidney transplant can restore a normal lifestyle and significantly extend lifespan (with 18-55% of kidneys still functioning after ten years). However, transplantation is complex, costly, and requires a compatible donor kidney from close relatives or a matched donor, which can be challenging to find. Meanwhile, patients may continue dialysis until a suitable donor is found. After transplantation, patients must take immunosuppressive medications (such as steroids, cyclosporine, and azathioprine) daily to prevent rejection of the new kidney.
If you suspect renal failure such as having fatigue, anemia, loss of appetite, nausea and vomiting, cramps in the hands and feet, swollen feet, or red and greenish spots on the skin, especially in elderly, people with chronic diseases (such as diabetes, high blood pressure, gout, or kidney disease), or a history of taking pain relievers or anti-inflammatory drugs for a long time, you should see a doctor.
Once diagnosed with renal failure, you should take care of yourself as follows:
- Follow your doctor's instructions for treatment, medication, and lifestyle changes.
- Continue to see your doctor as scheduled.
- Do not adjust your medication dosage or take medication on your own. Some medications can be toxic to the kidneys, and the dosage may need to be reduced from the usual dosage for normal people. Avoid herbal medicines, as they can increase blood potassium levels. Taking medication incorrectly can be dangerous.
See your doctor before your scheduled appointment if you experience any of the following:
- Fatigue, shortness of breath, loss of appetite, nausea and vomiting, swollen feet, cramps, lethargy, seizures, bleeding, or other discomfort (such as fever, abdominal pain, diarrhea, etc.)
- Run out of medication, lose your medication, or are unable to take your medication
- Suspect side effects from medication, such as hives, rash, blisters, swollen eyes, swollen mouth, abdominal pain, diarrhea, nausea, vomiting, red and greenish spots, or other unusual symptoms
1. Regularly check if you have high blood pressure, diabetes, or gout. If you do, it's crucial to treat these conditions seriously and continuously to maintain normal levels of blood pressure, blood sugar, and uric acid.
2. If you have a urinary tract infection (such as bladder inflammation or kidney inflammation) or a urinary tract obstruction (such as kidney stones or an enlarged prostate), you must get appropriate and complete treatment.
3. If you contract an infectious disease, suffer a snake bite, or experience diarrhea, seek treatment promptly. Do not let these conditions progress to shock, which can lead to renal failure.
4. Avoid using medications that may be toxic to the kidneys and be cautious with medication use in patients with poor kidney perfusion (such as those with cirrhosis, heart failure, renal artery stenosis, or shock due to decreased blood volume).
1. Patients with chronic renal failure should maintain regular contact with their doctor. Strict adherence to prescribed medications, diet, and lifestyle recommendations from your healthcare provider can help improve your quality of life and extend your lifespan.
2. Kidney failure is a condition with serious complications. Chronic renal failure is particularly complex and expensive to treat. Therefore, it is important to prevent this disease, especially in people with diabetes or high blood pressure. Serious management of these conditions can help control the diseases and reduce the risk of developing kidney failure.
3. Kidney transplantation is currently the best treatment for end-stage chronic renal failure. It is recommended that kidney donations be promoted to increase the availability of donor kidneys, which can relieve the suffering of patients and allow them to lead a normal quality of life.
Qualifications for Kidney Transplant Recipients
- Age not exceeding 55 years old. Older patients are less likely to benefit from surgery due to hardened blood vessels.
- No significant diseases such as heart disease, lung disease, liver disease, cancer, etc.
- No infectious diseases. After kidney transplantation, patients must take immunosuppressive drugs, which can exacerbate infectious diseases.
- Strong determination. After surgery, there may be many complications. Therefore, the patient must be prepared to fight any problems that may arise.
- Committed to maintaining good health and able to follow doctor's instructions, especially taking medication strictly.