Heart failure (or congestive heart failure) is a condition in which the heart muscle loses its ability to pump blood efficiently to supply various parts of the body. This loss of ability prevents tissues from receiving blood and adequate oxygen, leading to symptoms such as weakness and fatigue.
Heart failure can affect both the left and right heart chambers, but it most commonly occurs in the left, which is often followed by right-sided heart failure. Left-sided heart failure (usually caused by coronary artery disease, arrhythmia, cardiomyopathy, myocarditis, hypertension, etc.) can lead to fluid buildup in the lungs, known as "pulmonary edema," causing breathing difficulties or fatigue.
Right-sided heart failure usually follows left-sided heart failure. However, it can sometimes result from other factors (such as chronic obstructive pulmonary disease or abnormalities of the right heart chamber). This type of heart failure can cause fluid retention in the liver (resulting in an enlarged liver), abdomen (causing abdominal swelling), and limbs (swollen arms and legs).
Heart failure symptoms are typically chronic, a condition known as "chronic heart failure."
However, some patients may experience a sudden onset of symptoms, referred to as "acute heart failure." Myocardial infarction from a complete blockage of the heart's blood vessels is one common cause, known as a "heart attack," which can result in sudden death.
Heart failure is a serious condition that requires timely and continuous medical treatment. If treatments are delayed or the symptoms are left untreated, the condition usually worsens and becomes life-threatening.
This disease can be found in people of all ages but is more common in high-risk groups, including the elderly (over 65), obese individuals, those with diabetes or hypertension, smokers, heavy drinkers, and individuals with a family history of heart failure.
There are several possible reasons for heart failure, with prevalent factors including:
- Coronary artery disease and myocardial infarction, which are the most common causes of heart failure.
- Long-term untreated high blood pressure forced the heart to work harder, thickening the muscles in the lower left chamber and reducing its ability to pump blood.
- Myocarditis, often caused by viral infections, including COVID-19, can lead to left-sided heart failure.
- Arrhythmias, such as excessively slow or fast heart rhythms or irregular heartbeats.
- Valvular heart stenosis or regurgitation (from congenital defects or rheumatic heart disease) or congenital heart diseases (defective heart wall or valve) contribute to heart exhaustion and failure.
- Cardiomyopathy, in which the heart muscles enlarge and become weak, resulting in heart failure. Causes include chronic alcohol consumption, long-term substance abuse (such as cocaine or amphetamine), diabetes, high blood pressure, obesity, hyper- or hypothyroidism, COVID-19 infection, and autoimmune diseases (such as SLE or rheumatoid arthritis), among others.
- Chemotherapy and radiotherapy.
- Certain medications, such as antiarrhythmic drugs, non-steroidal anti-inflammatory drugs (NSAIDs), pioglitazone (diabetes medication), chloroquine (used in treating malaria), and itraconazole (antifungal drug).
- Other factors include heavy alcohol consumption, smoking, being overweight, diabetes, high cholesterol, hyperthyroidism or hypothyroidism, chronic renal failure, chronic obstructive pulmonary disease (e.g., emphysema), asthma, anemia, thiamine deficiency, and HIV infection. These conditions can alter heart structure (in coronary arteries or cardiac muscles) and functions (heart straining, inability to pump blood, or reduced pumping), causing heart failure.
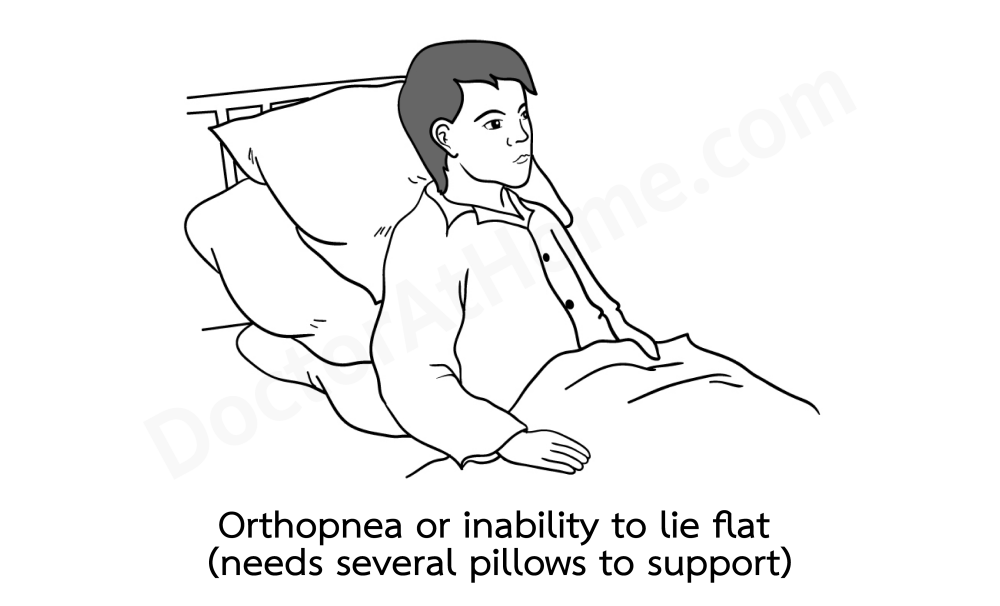
In the early stages, breathlessness and fatigue during exertion are common. Coughing and difficulty breathing when lying flat may occur, prompting the patient to sit up. Some experience wheezing similar to asthma and need to breathe in the air from outside to relieve the symptoms.
Patients may feel tightness or discomfort in the epigastric area (the upper central region of the stomach), pain around the right rib cage, and swollen hands or ankles.
In cases caused by coronary artery disease, there may be chest tightness.
As the condition progresses, shortness of breath and fatigue may worsen, occurring even with minimal activity or rest. Patients may need to rest on propped-up pillows. Reduced urine output is possible, as is increased nighttime urination. Swelling often affects the feet and legs and may extend to the abdomen. The face or eyes usually do not swell, as seen in patients with kidney disease.
Patients may gain weight rapidly due to edema (fluid retention) in various parts of the body.
In severe cases, there may be severe coughing with frothy, red-tinged mucus. Skin and lips may turn bluish. Restlessness and palpitations are possible. Urgent treatment is necessary to prevent death.
Most patients have chronic symptoms that gradually worsen over time.
In cases of acute heart failure, patients may experience severe shortness of breath, chest tightness, a feeling of suffocation, and extreme fatigue. Other signs include foot swelling, coughing or wheezing, chest pain, palpitations or irregular heartbeat, loss of appetite, nausea, cold extremities, bluish lips, dizziness, and loss of consciousness.
Some patients develop shock (caused by heart abnormalities, called "cardiogenic shock." This can be found in some acute heart failure patients, usually those with acute myocardial infarction).
Acute heart failure often occurs due to worsening of pre-existing chronic heart failure. In rare cases, sudden onset of symptoms might be triggered after an event, such as acute myocardial infarction, arrhythmia, acute myocarditis, hypertensive crisis, or pulmonary embolism.
Complications most likely to be found include:
- Arrhythmias, particularly atrial fibrillation, which can pose significant risks.
- Valvular heart disease, such as heart failure, causes the heart to enlarge, increases internal pressure, and leads to valve dysfunction.
- Chronic kidney disease, due to reduced blood flow to the kidneys, gradually damages the organ; in severe cases, dialysis may be necessary.
- Cirrhosis, due to increased pressure on liver cells from fluid retention, damages cells and impairs liver function.
- Pulmonary edema, resulting in breathing difficulty.
- Malnutrition contributes to decreased food intake and nutrient deficiencies due to symptoms such as nausea, loss of appetite, and abdominal fullness (resulting from abdominal swelling due to fluid retention).
Doctors will make an initial diagnosis based on symptoms, medical history, and physical examination.
Key findings include:
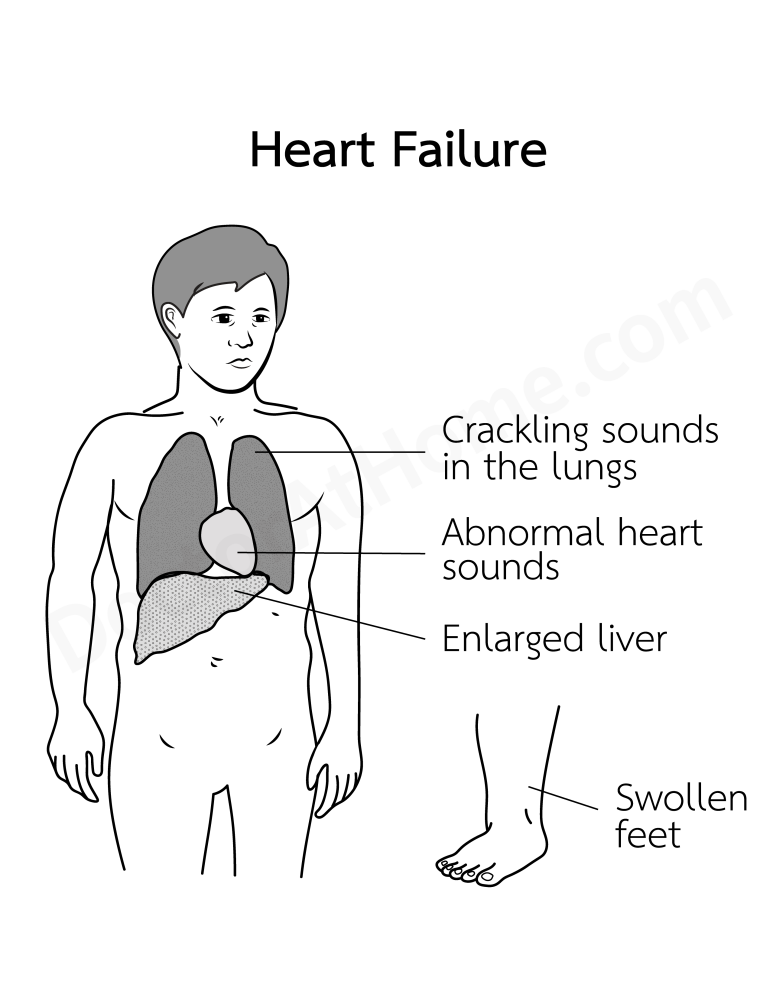
Shortness of breath. Difficulty breathing when lying flat. Bulging neck veins. Swelling in the hands and feet (a dent is left when applying pressure on the ankles). In some cases, fluid accumulation in the abdomen may be present.
Rapid heart rate or irregular heart rate in some patients.
Crackling sounds (crepitations) in both lungs, especially under the shoulder blades, on stethoscopic examination. In some instances, wheezing sounds (similar to asthma) may also be heard.
An enlarged liver is often detected on palpation.
A stethoscope may reveal irregular heartbeats or murmurs. Patients may have high blood pressure or other symptoms, depending on the underlying cause.
In patients with shock, sweating, cool skin, a weak, rapid pulse, and low blood pressure will be present.
Doctors will make a definitive diagnosis using tests such as blood tests (to check for anemia, complete blood count, liver and kidney function, thyroid function, blood sugar, lipids, electrolytes, and natriuretic peptide (BNP or NT pro-BNP, which are elevated in heart failure), urinalysis, chest X-ray, electrocardiogram, echocardiogram, cardiac MRI or CT scan, coronary angiogram, or myocardial biopsy (a small heart tissue sample is taken for lab analysis to diagnose specific heart muscle diseases that can cause heart failure).
Physicians will admit patients to the hospital for treatment and provide the following:
1. Acute heart failure treatment includes addressing respiratory failure with intubation, mechanical ventilation, or administering oxygen as indicated, managing fluid overload with diuretics (e.g., furosemide) and limiting fluid and sodium intake, and treating shock if present.
Additionally, physicians may consider other medications (to dilate blood vessels, increase heart contractions, or tighten blood vessels) and other treatment modalities as necessary for each patient.
2. Medications to control heart failure. There are several types of medications available, which are often used in combination:
(a) ACE inhibitors (e.g., enalapril, lisinopril, captopril) or ARBs (angiotensin II receptor blockers, e.g., losartan, valsartan) to reduce blood pressure, improve blood flow, and enhance heart function.
(b) Beta-blockers (e.g., bisoprolol, carvedilol) to slow down heart rate, lower blood pressure, and improve heart function.
(c) Mineralocorticoid receptor antagonists (MRAs, e.g., spironolactone) at low doses to counteract harmful changes in heart structure (such as cardiac fibrosis).
Physicians usually prescribe a combination of these three medications as a baseline treatment*. If the patient’s response is less than optimal, the treatment may be adjusted by adding other drugs (e.g., digoxin or ivabradine) or alternative medications, such as ANRIs (sacubitril/valsartan). If allergies or contraindications prevent the use of the medications above, physicians may consider prescribing hydralazine with isosorbide instead*.
For patients unresponsive to medication, options like implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) may be considered.
3. Treatment for underlying conditions contributing to heart failure, including:
- Managing diabetes, hypertension, high cholesterol, arrhythmias, chronic obstructive pulmonary disease, or anemia with appropriate medications.
- Using continuous positive airway pressure (CPAP) machines for sleep apnea.
- Surgery may be required for patients with congenital or rheumatic heart disease.
- Interventions like balloon angioplasty or coronary artery bypass surgery may be considered for patients with coronary artery disease.
4. For patients with end-stage heart failure (severe and unresponsiveness to treatment), physicians may consider mechanical circulatory support device implantation or heart transplantation.
The outcome of treatment depends on the cause and severity of the disease. Appropriate and continuous treatment will help reduce symptoms, complications, hospital readmissions, and the risk of death. However, severe, poorly managed heart failure, or heart failure caused by severe conditions, may lead to frequent exacerbations, repeated hospitalizations, or potential death.
*Reference: The Heart Association of Thailand under the Royal Patronage of H.M. the King. Heart Failure Council of Thailand (HFCT) 2019 Heart Failure Guideline, 2019.
If you have symptoms that are indicative of heart failure, such as fatigue and swollen feet, you should consult a doctor promptly.
Seek immediate medical attention if you have wheezing, difficulty breathing, severe chest pain, or fainting.
Once diagnosed with this condition, you should take care of yourself as follows:
1. Follow the doctor's advice for self-care practices and treatment.
2. Practice the following:
- Avoid alcohol and cigarettes.
- Avoid strenuous activities.
- Exercise, such as walking, according to your ability (discuss the appropriate level with your doctor).
- To control the disease, eat a healthy diet, focusing on vegetables, fruits, fish, tofu, nuts, and skimmed milk. Avoid sweet, fatty, and salty foods, as well as sugar, sugary drinks, red meat, and fatty meat.
- Limit the amount of water and sodium consumed daily (as advised by your doctor) to reduce swelling and prevent symptoms from worsening.
- Maintain a healthy weight.
- Track swelling in your feet and weigh yourself daily at home. If you notice changes or rapid weight gain, you should see a doctor promptly.
- Get enough rest and relaxation (via hobbies, watering plants, watching movies, listening to music, painting, meditation, enjoying nature and art, socializing, or participating in group therapy).
- Take medications exactly as prescribed by your doctor. Do not stop or adjust your medication (in category or dosage) without consulting your doctor first.
- Avoid self-medicating with medications, herbs, or dietary supplements, as these can exacerbate the disease or interact negatively with your current medications.
- Get vaccinations as recommended by your doctor, such as COVID-19, influenza, and pneumonia.
3. You should return to your doctor before the scheduled appointment if you have any of the following issues:
- Tiredness, shortness of breath when lying down, swelling in the abdomen or extremities, extreme fatigue, or rapid weight gain.
- Symptoms such as high fever, severe abdominal pain, frequent diarrhea, frequent vomiting, or paleness.
- Snoring and daytime sleepiness, or possible sleep apnea.
- Missed medication doses, lost medication, or suspected side effects from medication or drug allergies.
You can significantly reduce your risk of heart failure by taking the following steps:
- Engage in regular physical activity.
- Quit smoking.
- Avoid drinking alcohol (If necessary, only drink in moderate amounts)
- Adopt a healthy diet, especially one that includes fruits, vegetables, tofu, grains, and nuts. Minimize sugar, sweetened food, unhealthy fats, and salt.
- Achieve and maintain a healthy weight range.
- Prioritize enough sleep and utilize stress-management techniques.
- Treat underlying risk factors for heart failure, such as coronary artery disease, diabetes, high blood pressure, and hyperthyroidism.
- Prevent the recurrence of heart failure symptoms by carefully following your doctor's treatment plan and lifestyle advice.
1. Heart failure is a chronic condition requiring continuous care. It may have frequent aggravations, severe complications, and potentially sudden death within 5-10 years after the first manifestation of symptoms. Patients need to check up with their doctors routinely and practice self-treatment regularly.
Patients and their loved ones should learn about the nature of heart failure and apply appropriate self-care practices in daily life. These practices will maximize the patient’s quality of life and longevity.
2. Individuals with non-communicable chronic diseases (including heart disease, diabetes, high blood pressure, high cholesterol, pulmonary emphysema, chronic kidney disease, or autoimmune diseases) or risk factors (such as obesity, smoking, or excessive alcohol use) should actively manage these conditions, modify behaviors to reduce risk factors and monitor any symptoms. If heart failure is suspected, consulting a doctor promptly for a timely examination and treatment can significantly improve outcomes.