Ischemic Heart Disease (IHD), also known as Coronary Artery Disease (CAD), refers to the narrowing or blockage of coronary arteries due to plaque buildup. This condition can lead to reduced blood flow to the heart muscle, causing various symptoms and complications. CAD can be classified into two main types: chronic (Stable Ischemic Heart Disease) and acute (Acute Coronary Syndromes).
Types of CAD
1. Chronic Coronary Artery Disease (also known as Stable Ischemic Heart Disease)
This type is characterized by predictable chest pain or discomfort (stable angina) that occurs during physical exertion or stress and is typically relieved by rest or medication. The primary cause is the gradual accumulation of plaques in the coronary arteries, which restricts blood flow but does not completely block it.
2. Acute Coronary Syndromes (ACS)
ACS encompasses conditions that result from a sudden and severe reduction in blood flow to the heart, leading to more urgent and severe symptoms. It includes:
- Unstable Angina: A life-threatening emergency characterized by new or worsening chest pain that can occur even at rest. Unlike stable angina, this pain is not relieved by rest or medication and typically worsens over time, indicating an increased risk of an imminent heart attack.
- Non-ST-Elevation Myocardial Infarction (NSTEMI): A type of heart attack characterized by heart muscle damage without the classic elevation in the ST segment on an ECG. Despite the absence of this specific ECG change, NSTEMI is a life-threatening emergency that requires immediate medical attention.
- ST-Elevation Myocardial Infarction (STEMI): A severe heart attack where a coronary artery is completely blocked, leading to significant heart muscle damage. It is characterized by elevated ST segments on an ECG and is a life-threatening emergency that requires immediate medical attention.
IHD or CAD involves the narrowing or blockage of coronary arteries, primarily due to atherosclerosis. This condition can manifest as either a chronic problem or an acute event.
Chronic Coronary Artery Disease is driven by long-term risk factors like high cholesterol, hypertension, smoking, diabetes, and sedentary lifestyles. These contribute to the gradual buildup of plaques, leading to stable angina with predictable symptoms during exertion.
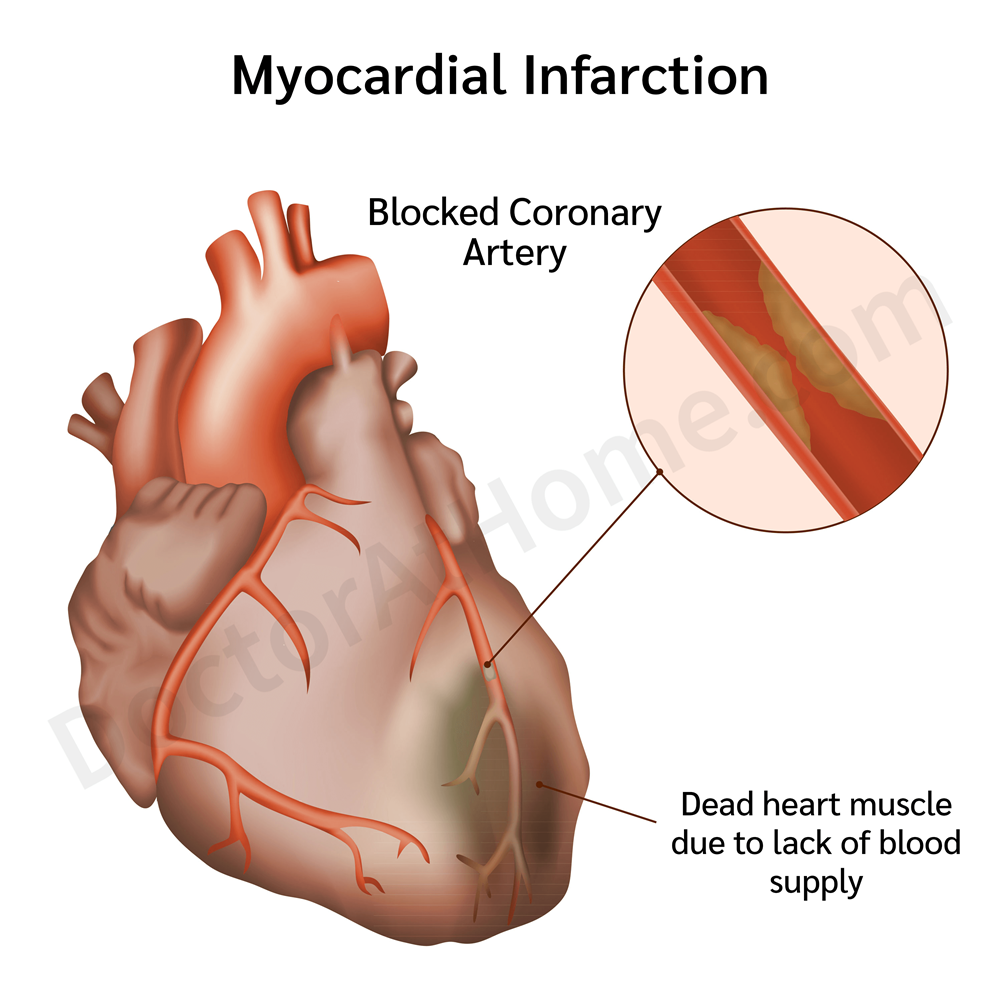
Acute Coronary Syndromes include conditions like unstable angina and myocardial infarction. Unstable angina results from partial blockages or severe spasms, indicating an imminent risk of heart attack. Myocardial infarction involves complete arterial blockages due to plaque rupture and clot formation, leading to significant heart muscle damage.
1. Chronic Coronary Artery Disease (Stable Ischemic Heart Disease)
Chronic CAD or Stable IHD develops gradually due to persistent risk factors that contribute to the buildup of plaques within the coronary arteries. These plaques slowly narrow the arteries, reducing blood flow to the heart muscle over time.
Key Causes and Risk Factors:
- Atherosclerosis:
- Process: Over time, fats, cholesterol, and other substances accumulate on the arterial walls, forming plaques. These plaques harden and narrow the arteries, a condition known as atherosclerosis.
- Effect: The gradual narrowing limits blood flow, leading to symptoms such as chest pain during physical exertion.
- High Cholesterol Levels:
- LDL Cholesterol: Elevated low-density lipoprotein (LDL) cholesterol, known as “bad” cholesterol, contributes to plaque buildup in the arteries.
- HDL Cholesterol: Low levels of high-density lipoprotein (HDL) cholesterol, the “good” cholesterol, which helps clear cholesterol from the bloodstream, can also increase risk.
- High Blood Pressure (Hypertension):
- Damage: Consistently high blood pressure can damage the inner lining of arteries, making them more susceptible to atherosclerosis.
- Increased Heart Load: It forces the heart to work harder, accelerating plaque accumulation.
- Smoking:
- Vascular Damage: Chemicals in tobacco smoke damage the coronary arteries' lining, promoting plaque buildup.
- Reduced Oxygen: Smoking reduces the oxygen-carrying capacity of the blood, increasing the heart’s workload.
- Diabetes:
- Increased Atherosclerosis: High blood sugar levels contribute to the development and acceleration of atherosclerosis by damaging blood vessels.
- Inflammation: Diabetes is associated with inflammation and higher cholesterol levels, both of which exacerbate CAD.
- Obesity:
- Contributing Factors: Excess body weight is linked to high cholesterol, high blood pressure, and diabetes, all of which are risk factors for CAD.
- Heart Strain: Obesity increases the heart’s workload, exacerbating the impact of narrowed arteries.
- Physical Inactivity:
- Impact: A lack of physical activity is associated with poor blood circulation, high cholesterol, and high blood pressure, which contribute to plaque buildup.
- Low HDL Levels: Inactivity is linked to lower levels of HDL cholesterol, which helps remove LDL cholesterol from the arteries.
- Unhealthy Diet:
- Dietary Risks: Diets high in saturated fats, trans fats, and sodium contribute to high cholesterol and high blood pressure, promoting atherosclerosis.
- Family History of Heart Disease:
- Genetics: A family history of heart disease increases the likelihood of developing atherosclerosis and CAD.
- Shared Habits: Family members often share lifestyle factors that contribute to risk.
2. Acute Coronary Syndromes (ACS)
ACS events, which include unstable angina and myocardial infarction (heart attack), are typically caused by sudden disruptions in blood flow to the heart. These can result from the rapid formation of blood clots due to plaque rupture or severe artery spasm.
- Unstable Angina
- Plaque Disruption:
- Partial Blockage: Unstable angina often occurs when a plaque in the coronary artery ruptures or erodes. This causes the formation of a blood clot that partially obstructs blood flow.
- Intermittent Symptoms: The resulting blockage is not complete, leading to chest pain at rest or with minimal exertion, and is a warning sign of a potential heart attack.
- Coronary Artery Spasm:
- Temporary Constriction: Unstable angina can also be triggered by a sudden, intense spasm of a coronary artery, which temporarily reduces or blocks blood flow to the heart muscle.
- Triggers: Common triggers for spasms include stress, smoking, and exposure to cold.
- Severe Plaque Narrowing:
- Advanced Atherosclerosis: As atherosclerosis progresses, plaques can narrow the arteries to a critical point where even a minor increase in plaque size or blood clot can significantly reduce blood flow.
- High Risk of Heart Attack: This severe narrowing raises the risk of a heart attack.
- Myocardial Infarction (Heart Attack)
- Plaque Rupture and Complete Thrombus Formation:
- Total Blockage: Myocardial infarction typically occurs when plaque in a coronary artery ruptures, causing a large blood clot to form that completely blocks the artery. This prevents blood from reaching parts of the heart muscle, leading to tissue death.
- Irreversible Damage: The longer the artery remains blocked, the greater the damage to the heart muscle, making immediate treatment critical.
- Coronary Artery Spasm:
- Prolonged Spasm: A severe and prolonged spasm of a coronary artery can also cause a myocardial infarction by cutting off blood flow long enough to damage the heart muscle.
- Risk Factors: Triggers for severe spasms can include drug use, extreme stress, or cold exposure.
- Rapid Progression of Atherosclerosis:
- Sudden Plaque Growth: Rapid accumulation or destabilization of plaques can quickly narrow the coronary arteries to a critical level, precipitating an acute event.
1. Chronic CAD (Stable Ischemic Heart Disease)
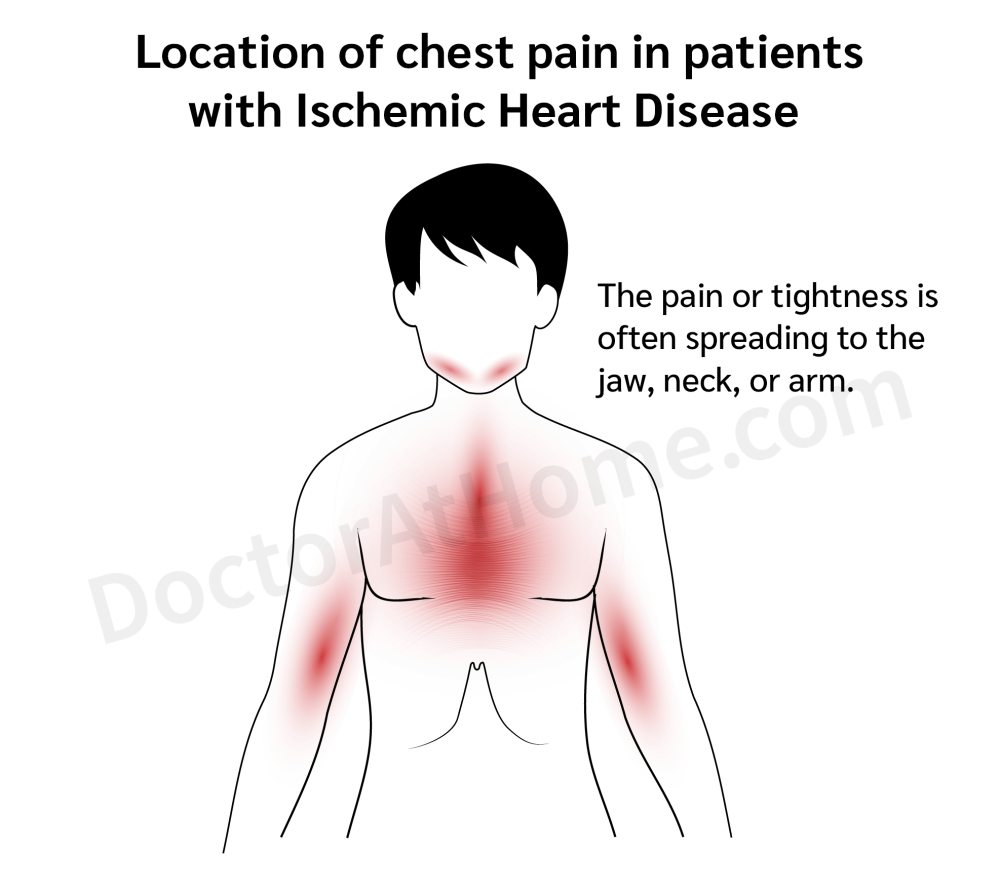
- Chest pain or discomfort (angina): Often described as pressure, heaviness, or tightness, typically triggered by physical activity or stress and relieved by rest. Chest pain or discomfort typically lasts for 1 to 5 minutes but can persist up to 15 minutes. This pain usually subsides after resting or stopping the activity that triggered it, or after taking vasodilator medication, such as nitroglycerin. Some cases may also experience pain radiating to the neck, jaw, back, or one or both arms.
- Shortness of breath: Especially during exertion or exercise.
- Fatigue: Feeling unusually tired, even with normal activities.
- Predictable pattern: Symptoms follow a consistent pattern and are generally manageable with lifestyle adjustments and medications.
- Less known symptoms: In many instances, some people may not feel chest pain at all. Instead, they might experience discomfort or pain in other parts of their body.
Commonly affected areas include the jaw, teeth, shoulders, arms, neck, or back. This occurrence is due to a phenomenon called referred pain, where pain signals from the heart are felt in other regions of the body. For example, pain in the jaw or teeth might be mistaken for dental problems, and discomfort in the shoulders or arms could be incorrectly attributed to musculoskeletal problems. These variations in pain presentation can sometimes delay the diagnosis of ischemic heart disease, as patients and healthcare providers may not immediately link these symptoms to a heart condition.
Recognizing that ischemic heart disease can manifest through pain in diverse parts of the body is vital for prompt and accurate diagnosis. If individuals experience unexplained pain in these areas, especially when combined with shortness of breath, nausea, sweating, or lightheadedness, it is important to seek medical attention to rule out potential heart-related issues.
2. Acute Coronary Syndromes (ACS)
- Unstable Angina:
- Chest pain at rest: Sudden and severe chest pain that occurs without exertion and doesn’t subside with rest or medication.
- High risk of heart attack: Indicates a significant increase in the risk of progressing to a myocardial infarction. In cases of myocardial infarction, many will experience intense, continuous chest pain lasting for hours or days, unrelieved by rest, similar to but more severe than angina pectoris. Symptoms often include weakness, fatigue, palpitations, dizziness, nausea, vomiting, and sometimes shortness of breath from heart failure or shock. Some may feel abdominal tightness like gastritis or have had chest pain in the weeks prior, while others may have silent heart attacks with no symptoms before the event. Severe cases may lead to fainting or sudden death.
- NSTEMI:
- Prolonged chest pain: Persistent chest pain or discomfort that doesn't go away with rest.
- Partial blockage: A coronary artery is partially blocked, causing some damage to the heart muscle.
- STEMI:
- Intense, severe chest pain: Persistent and severe pain indicating a complete blockage of a coronary artery.
- Significant damage: Requires immediate medical intervention to restore blood flow and limit heart muscle damage.
Less known symptoms: Just like Chronic CAD, in many instances, some people may not feel chest pain at all. Instead, they might experience discomfort or pain in other parts of their body.
Without proper management, IHD or CAD can lead to serious and potentially life-threatening complications.
1. Chronic CAD (Stable Ischemic Heart Disease)
- Heart Failure: Chronic reduced blood flow can weaken the heart muscle, leading to its inability to pump blood effectively.
- Arrhythmias: Irregular heartbeats due to damaged or scarred heart tissue.
- Persistent Chest Pain: Ongoing angina that can limit daily activities and decrease quality of life.
2. Acute Coronary Syndromes (ACS)
- Heart Attack (Myocardial Infarction): A complete or significant blockage leading to the death of heart muscle cells and causing severe heart damage.
- Cardiogenic Shock: A critical condition where the heart suddenly can’t pump enough blood to meet the body's needs.
- Sudden Cardiac Arrest: The heart stops abruptly, which can be fatal without immediate medical intervention.
For Chronic CAD (Stable Ischemic Heart Disease), the diagnosis focuses on assessing long-term effects of reduced blood flow and identifying blockages causing predictable symptoms through non-emergency tests. For Acute Coronary Syndromes (ACS), the diagnosis is urgent, aiming to rapidly identify and treat severe or total blockages causing acute symptoms or heart attacks through immediate and intensive evaluation.
1. Chronic Coronary Artery Disease (Stable Ischemic Heart Disease)
For diagnosing chronic CAD, the focus is on identifying the underlying atherosclerosis and assessing how it impacts heart function over time. The following methods are commonly used:
Medical History and Physical Examination
- Purpose: To gather comprehensive information about symptoms, risk factors, and medical history.
- Details: Doctors will ask about the frequency, duration, and triggers of chest pain or discomfort, along with lifestyle factors such as diet, exercise, smoking, and family history of heart disease.
Electrocardiogram (ECG/EKG)
- Purpose: To measure the heart’s electrical activity and detect abnormalities.
- Details: An ECG can reveal patterns indicating past or ongoing ischemia and assess the heart's rhythm and electrical activity at rest.
Stress Testing
- Purpose: To evaluate how the heart performs under physical stress.
- Details: During a treadmill or bicycle exercise test, the heart’s response is monitored through ECG. If the patient cannot exercise, medications may be used to simulate the effects of physical exertion.
Echocardiogram
- Purpose: To use ultrasound to visualize heart structure and function.
- Details: An echocardiogram assesses the size, shape, and motion of the heart's chambers and valves. It helps detect areas with poor blood flow or damage from previous heart attacks.
Coronary Angiography
- Purpose: To visualize the coronary arteries directly.
- Details: A contrast dye is injected into the coronary arteries, and X-ray imaging is used to identify blockages or narrowings in the arteries.
CT Coronary Angiography
- Purpose: To provide detailed images of the coronary arteries non-invasively.
- Details: This test uses CT scanning to create high-resolution images, which can help evaluate the severity and location of blockages in patients at intermediate risk.
Blood Tests
- Purpose: To assess risk factors and guide long-term management strategies.
- Details: Blood tests such as the lipid profile, High-Sensitivity C-Reactive Protein, fasting blood glucose, Fasting Blood Glucose and Hemoglobin A1c, homocysteine, and Lipoprotein (a) are primarily used for this purpose.
2. Acute Coronary Syndromes (ACS)
Diagnosing ACS focuses on quickly identifying and treating significant or total blockages in the coronary arteries that can cause severe symptoms or heart attacks. The diagnostic steps include:
Immediate Medical Assessment
- Purpose: To rapidly evaluate symptoms and determine the severity of the condition.
- Details: Emergency assessment involves checking vital signs and reviewing symptoms like severe chest pain, shortness of breath, and signs of heart failure or shock.
Electrocardiogram (ECG/EKG)
- Purpose: A critical initial test to detect ST-segment elevation or other changes.
- Details: An ECG is performed immediately to identify the type of ACS (e.g., STEMI, NSTEMI) based on electrical patterns in the heart.
Cardiac Biomarker Tests
- Purpose: To detect enzymes and proteins that are released when heart muscle is damaged.
- Details: Blood tests measure levels of cardiac biomarkers like troponin, which rise within hours after a heart attack, helping confirm the diagnosis and severity.
Coronary Angiography
- Purpose: To visualize and treat blockages in coronary arteries.
- Details: Often performed urgently to identify and clear blockages in the arteries during NSTEMI or STEMI, guiding decisions for interventions like angioplasty or bypass surgery.
Chest X-ray
- Purpose: To assess the condition of the heart and lungs.
- Details: A chest X-ray helps rule out other causes of symptoms, such as aortic dissection or pulmonary issues, and evaluates the size of the heart and fluid around it.
Echocardiogram
- Purpose: To provide real-time images of heart function.
- Details: An echocardiogram is used in emergency settings to quickly assess heart function, detect areas of muscle damage, and identify complications.
Blood Tests
- Purpose: To diagnose acute cardiac events and determining the extent of heart muscle damage.
- Details: Troponin levels, Creatine Kinase-MB, myoglobin, and B-Type Natriuretic Peptide or N-Terminal proBNP is crucial for diagnosing.
1. Chronic Coronary Artery Disease (Stable Ischemic Heart Disease)
Chronic CAD (Stable Ischemic Heart Disease) is managed with a combination of medications (antiplatelets, statins, beta-blockers, nitrates, calcium channel blockers, and ACE inhibitors/ARBs) and procedures like PCI or CABG to maintain and restore blood flow.
1. Medications:
- Antiplatelet Agents: Aspirin or clopidogrel (Plavix) are used to prevent blood clots and reduce the risk of heart attack.
- Statins: Drugs like atorvastatin (Lipitor) and simvastatin (Zocor) lower cholesterol levels and stabilize plaques in the arteries.
- Beta-Blockers: Medications such as metoprolol (Lopressor) and atenolol (Tenormin) reduce heart rate and blood pressure, lowering the heart’s oxygen demand.
- Nitrates: Nitroglycerin is used to dilate blood vessels and relieve chest pain.
- Calcium Channel Blockers: Amlodipine (Norvasc) and diltiazem (Cardizem) help relax blood vessels, improving blood flow and reducing chest pain.
- ACE Inhibitors/ARBs: Lisinopril (Prinivil) and losartan (Cozaar) lower blood pressure and reduce the heart's workload.
2. Procedures:
- Percutaneous Coronary Intervention (PCI): Also known as angioplasty, this procedure involves using a balloon to open a narrowed artery and placing a stent to keep it open.
- Coronary Artery Bypass Grafting (CABG): Surgical procedure to bypass blocked coronary arteries using a graft from another part of the body, improving blood flow to the heart.
2. Acute Coronary Syndromes (Unstable Angina and Myocardial Infarction)
Acute CAD (Unstable Angina and Myocardial Infarction) requires immediate intervention with medications (antiplatelets, nitroglycerin, anticoagulants, thrombolytics, beta-blockers, and pain relievers) and procedures (emergency PCI or CABG) to stabilize the patient and restore blood flow quickly.
1. Unstable Angina
- Medications:
- Antiplatelet Drugs: Aspirin and clopidogrel help prevent further clot formation.
- Nitroglycerin: Administered to quickly relieve chest pain by dilating the coronary arteries.
- Anticoagulants: Drugs like heparin or enoxaparin are used to thin the blood and prevent clotting.
- Beta-Blockers: These reduce heart rate and oxygen demand, easing the workload on the heart.
- Procedures:
- Percutaneous Coronary Intervention (PCI): Emergency PCI is often performed to reopen blocked coronary arteries and restore blood flow.
2. Myocardial Infarction (Heart Attack)
- Medications:
- Thrombolytics: Drugs like alteplase (Activase) or tenecteplase (TNKase) are used to dissolve blood clots blocking the coronary artery.
- Antiplatelet Agents: Aspirin and clopidogrel to prevent further clot formation.
- Beta-Blockers: Reduce heart rate and blood pressure to decrease the heart's oxygen demand.
- Pain Relievers: Morphine is often used to manage severe chest pain and reduce anxiety.
- Procedures:
- Percutaneous Coronary Intervention (PCI): Performed to quickly restore blood flow by opening the blocked artery.
- Coronary Artery Bypass Grafting (CABG): In cases where multiple arteries are blocked or PCI is not suitable, bypass surgery is performed.
1. Chronic Coronary Artery Disease (Stable Ischemic Heart Disease)
Chronic CAD involves long-term management to prevent disease progression and manage symptoms.
1. Adopt a Heart-Healthy Diet:
- Focus on Nutrient-Rich Foods: Incorporate plenty of fruits, vegetables, whole grains, and lean proteins.
- Limit Unhealthy Fats and Sodium: Reduce intake of saturated and trans fats, cholesterol, and salt to lower blood pressure and cholesterol levels.
- Balanced Meals: Aim for meals that include a variety of nutrients to support heart health.
2. Stay Physically Active:
- Regular Exercise: Engage in at least 150 minutes of moderate aerobic exercise, like walking or cycling, each week.
- Strength Training: Include activities that build muscle strength on at least two days per week.
- Personalized Plan: Consult with your doctor before starting any new exercise regimen.
3. Quit Smoking:
- Seek Help: Use resources such as nicotine replacement therapy, support groups, or counseling to quit smoking.
- Avoid Secondhand Smoke: Minimize exposure to secondhand smoke as it also increases the risk of CAD.
4. Manage Stress:
- Practice Relaxation Techniques: Engage in activities such as deep-breathing exercises, meditation, or yoga to reduce stress.
- Ensure Adequate Sleep: Aim for 7-9 hours of sleep per night to help the body manage stress better.
- Social Support: Maintain strong social connections to help cope with stress and improve emotional well-being.
5. Monitor Your Health:
- Regular Health Check-Ups: Keep up with scheduled visits to your doctor to monitor cholesterol, blood pressure, and blood sugar levels.
- Adhere to Medications: Follow your medication regimen as prescribed and report any side effects to your doctor.
- Symptom Awareness: Pay attention to changes in symptoms and seek medical advice if new issues arise.
- Reach out to your doctor if you experience any of the following:
- Irregularly fast or slow heartbeat
- Chest pain (angina) even when you are at rest
- Frequent stable angina
- Frequent lightheadedness, dizziness, palpitations, or fainting
- Seek Emergency Care if you experience any of the following:
- Your chest pain does not improve after taking three doses of nitroglycerin, with five-minute intervals between each dose.
- Your chest pain returns or becomes more intense.
- You notice a different type of chest pain than what you usually experience.
2. Acute Coronary Syndromes (Unstable Angina and Myocardial Infarction)
Acute Coronary Syndromes events, such as unstable angina or myocardial infarction, require immediate medical attention followed by specific self-care practices to support recovery and prevent recurrence.
1. Recognize Emergency Symptoms:
- Act Quickly: If you experience severe chest pain, shortness of breath, or other heart attack symptoms, seek emergency medical care immediately.
- Know the Signs: Learn the symptoms of a heart attack and unstable angina to respond promptly.
- Return to the doctor before your scheduled appointment if you experience any of the following:
- Recurring chest tightness or pain, feeling weak, tired easily, or swollen feet.
- Epigastric discomfort similar to gastritis that does not improve with medication for gastritis.
- Feeling unwell, such as having a high fever, severe stomach pain, severe diarrhea, severe vomiting, or looking pale.
- Suspect side effects from medication, such as hives, itchy rash, blisters, swollen eyes, swollen mouth, nausea, vomiting, red or bruised spots, or other unusual symptoms.
- Lost or ran out of medications.
2. Follow Post-Hospitalization Care:
- Take Medications as Prescribed: Continue all medications given after hospitalization to manage heart health and prevent further issues.
- Participate in Cardiac Rehabilitation: Engage in a structured rehab program to improve strength and learn about heart-healthy living.
- Monitor for Recurrence: Keep track of any recurring symptoms and seek immediate medical help if they appear.
3. Implement Lifestyle Changes:
- Heart-Healthy Diet: Continue to eat foods that support heart health and avoid foods high in unhealthy fats, sugars, and sodium.
- Gradual Return to Activity: Follow your doctor’s advice on resuming physical activities, starting slowly and increasing gradually.
- Avoid Tobacco and Alcohol: Quit smoking and limit alcohol intake to reduce the risk of further heart complications.
4. Support Emotional Health:
- Seek Counseling: Join support groups or consider therapy to help cope with the emotional impact of a heart attack.
- Stay Connected: Maintain strong relationships and social interactions for emotional support.
- Focus on Recovery: Set small, achievable goals to make positive changes in your lifestyle and heart health.
1. Prevention of Chronic Coronary Artery Disease (Stable Ischemic Heart Disease)
Prevention focuses on long-term lifestyle changes such as healthy eating, regular exercise, quitting smoking, managing stress, and monitoring key health indicators.
1. Healthy Diet:
- Balanced Nutrition: Emphasize a diet rich in fruits, vegetables, whole grains, and lean proteins. Avoid processed foods high in sugars and unhealthy fats.
- Limit Fats and Cholesterol: Reduce intake of saturated fats and trans fats, which can lead to plaque buildup in arteries.
- Control Sodium: Keep salt intake low to help manage blood pressure.
2. Regular Physical Activity:
- Consistent Exercise: Aim for at least 150 minutes of moderate aerobic activity each week, such as brisk walking, swimming, or cycling.
- Strength Training: Incorporate muscle-strengthening exercises on two or more days a week.
- Consult Doctors: Especially important for individuals with existing health conditions before starting new exercise routines.
3. Maintain a Healthy Weight:
- Weight Management: Achieve and maintain a healthy weight to reduce strain on the heart.
- Caloric Balance: Balance calorie intake with physical activity to manage weight effectively.
4. Avoid Smoking and Limit Alcohol:
- Quit Smoking: Seek support to stop smoking, which significantly reduces the risk of developing CAD.
- Limit Alcohol: If you drink, do so in moderation—up to one drink a day for women and two for men.
5. Manage Stress:
- Stress Reduction Techniques: Practice mindfulness, meditation, or yoga to manage stress levels.
- Healthy Coping Mechanisms: Engage in hobbies, social activities, and relaxation techniques to reduce stress.
6. Regular Health Screenings:
- Monitor Key Health Metrics: Regularly check blood pressure, cholesterol levels, and blood sugar.
- Follow Medical Advice: Adhere to your doctor's recommendations for managing any chronic conditions like hypertension or diabetes.
2. Prevention of Acute Coronary Syndromes (Unstable Angina and Myocardial Infarction)
Prevention involves strict adherence to prescribed medications, participation in rehabilitation programs, and ongoing health monitoring.
1. Medication Adherence:
- Follow Prescriptions: Take medications as prescribed to control risk factors and prevent acute events.
- Review with Your Doctor: Regularly review your medication regimen with your doctor to ensure it remains effective.
2. Lifestyle Changes Post-Event:
- Rehabilitation Programs: Participate in cardiac rehabilitation to regain strength and learn heart-healthy behaviors.
- Gradual Resumption of Activities: Follow a structured plan to return to regular activities safely and gradually.
3. Continuous Monitoring:
- Track Symptoms: Keep a log of any recurring symptoms and discuss them with your doctor.
- Regular Check-Ups: Schedule and attend follow-up appointments to monitor your heart health.
1. Chronic Coronary Artery Disease (Stable Ischemic Heart Disease)
Focuses on lifestyle changes, such as a healthy diet, regular exercise, quitting smoking, managing stress, and consistent health monitoring.
1. Adopt a Heart-Healthy Lifestyle:
- Balanced Diet: Focus on eating a variety of nutrient-rich foods, including fruits, vegetables, whole grains, and lean proteins. Limit intake of saturated fats, trans fats, and sodium.
- Regular Physical Activity: Engage in at least 150 minutes of moderate aerobic exercise per week, such as walking, swimming, or cycling. Include strength training exercises twice a week.
- Quit Smoking: Seek support to stop smoking, including nicotine replacement therapies and counseling. Avoid secondhand smoke as well.
2. Manage Stress:
- Practice Relaxation Techniques: Activities such as meditation, yoga, or deep-breathing exercises can help manage stress and improve heart health.
- Maintain Social Connections: Engage with friends and family to build a support network that helps reduce stress.
3. Monitor Your Health Regularly:
- Blood Pressure and Cholesterol Levels: Keep track of these vital indicators and manage them through diet, exercise, and medication as prescribed.
- Follow Up with Doctors: Schedule regular check-ups to monitor heart health and adjust treatment plans as necessary.
- Reach out to your doctor if you experience any of the following:
- Irregularly fast or slow heartbeat
- Chest pain (angina) even when you are at rest
- Frequent stable angina
- Frequent lightheadedness, dizziness, palpitations, or fainting
- Seek Emergency Care if you experience any of the following:
- Your chest pain does not improve after taking three doses of nitroglycerin, with five-minute intervals between each dose.
- Your chest pain returns or becomes more intense.
- You notice a different type of chest pain than what you usually experience.
4. Medication Adherence:
- Take Prescribed Medications: Consistently follow your medication regimen to manage risk factors such as high blood pressure, cholesterol, and blood sugar.
- Discuss Side Effects with Your Doctor: Regularly review your medications with your doctor to ensure they are effective and adjust as needed.
2. Acute Coronary Syndromes (Unstable Angina and Myocardial Infarction)
Emphasizes recognizing emergency symptoms, adhering to post-hospitalization care, gradually resuming activities, and ongoing health monitoring to prevent recurrence.
1. Recognize and Act on Emergency Symptoms:
- Act Quickly: If you experience severe chest pain, shortness of breath, or other heart attack symptoms, seek emergency medical care immediately.
- Know the Signs: Learn the symptoms of a heart attack and unstable angina to respond promptly.
- Return to the doctor before your scheduled appointment if you experience any of the following:
- Recurring chest tightness or pain, feeling weak, tired easily, or swollen feet.
- Epigastric discomfort similar to gastritis that does not improve with medication for gastritis.
- Feeling unwell, such as having a high fever, severe stomach pain, severe diarrhea, severe vomiting, or looking pale.
- Suspect side effects from medication, such as hives, itchy rash, blisters, swollen eyes, swollen mouth, nausea, vomiting, red or bruised spots, or other unusual symptoms.
- Lost or ran out of medications.
2. Follow Post-Hospitalization Care:
- Adhere to Medications: Continue all medications prescribed after hospitalization to prevent further complications and manage heart health.
- Participate in Cardiac Rehabilitation: Engage in a structured program to improve physical fitness, adopt healthy habits, and reduce the risk of future heart issues.
3. Gradual Return to Activities:
- Resume Activities Slowly: Follow your doctor’s guidelines for gradually increasing physical activity levels after an acute event.
- Monitor Your Symptoms: Keep track of any new or recurring symptoms and report them to your doctor.
4. Ongoing Health Monitoring:
- Regular Follow-Up Appointments: Schedule and attend follow-up visits to monitor your heart’s recovery and adjust treatments as needed.
- Continuous Health Assessments: Keep an eye on key health indicators like blood pressure, cholesterol, and glucose levels to ensure they remain within target ranges.