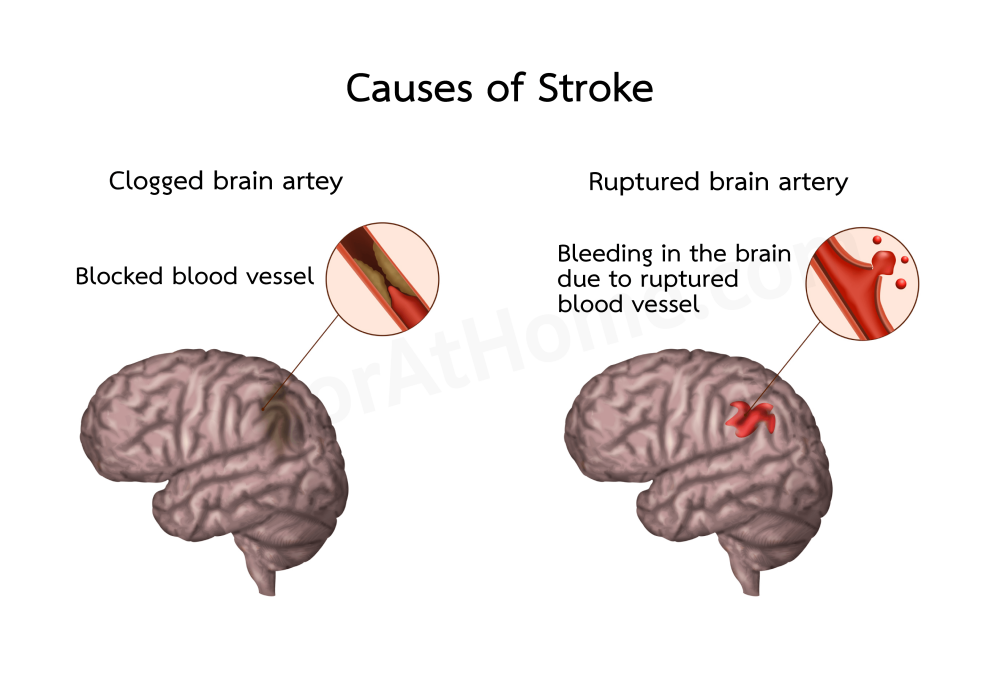
This condition results from abnormalities in the brain's arteries, such as narrowing, blockage, or rupture, causing some parts of the brain that control the body's functions to die and stop working. This results in paralysis of the affected body parts.
Symptoms usually occur suddenly and are referred to as cerebrovascular accidents or brain attacks.
*Paralysis means weakness of the limbs or other external organs (such as face, eyes, mouth), causing those body parts to be immobile or less mobile than usual, which may or may not be accompanied by a numbness (lack of pain).
If both legs are weak or immobile, it is called paraplegia. If all four limbs are immobile, it is called quadriplegia. These types of paralysis are often caused by spinal conditions (acute spinal cord inflammation, spinal cord injury, or a spinal cord tumor).
However, if only one side of the limbs is weak or immobile, it is called hemiplegia, which will be discussed here.
For other types of paralysis symptoms, please see "Paralysis/Weak limbs/Drooping eyelid."
1.) Ischemic stroke, which accounts for about 80% of stroke cases, is divided into two subtypes:
This disease is often found in people with high blood pressure, diabetes, high blood cholesterol, or a history of smoking, which can lead to this condition before old age because these people tend to have hardened arteries faster than normal.
In addition, older individuals (≥ 55 years in men and 65 years in women), heavy alcohol drinkers, women who use birth control pills (especially if they also smoke), those who are obese or overweight, individuals lacking physical exercise, those with sleep apnea, and people with a family history of hemiplegia are at a higher risk of developing this disease.
Thrombotic stroke is the most common cause of stroke or hemiplegia and is less dangerous than hemorrhagic stroke.
In addition to abnormalities in the arteries in the brain, ischemic stroke is also found in approximately 10-15% of stroke patients due to abnormalities in the arteries in the neck or carotid arteries, which are responsible for supplying blood to the brain.
(2) Embolic stroke is caused by an "embolus," which is a blood clot that forms in a blood vessel outside the brain (commonly in the carotid artery and heart) and travels through the bloodstream to block a blood vessel that supplies blood to the brain, causing brain cells to die due to lack of blood. It is often found in patients with carotid artery disease and heart disease (such as atrial fibrillation, rheumatic heart disease, myocardial infarction, congenital heart disease, endocarditis, heart valve disease, patients with artificial heart valves, etc.). In addition, it may also be found in patients with polycythemia and patients with bone marrow embolism (which occurs in patients with fractures).
2. Cerebral hemorrhage/Hemorrhagic stroke causes the surrounding brain tissue to die and accounts for about 20% of acute strokes. It is a serious condition that can lead to death quickly. The average mortality rate is 40-50%.
In the elderly, it is often caused by high blood pressure.
As the plaque or atheroma thickens, it narrows the arteries, reducing the blood supply to various organs (such as the heart, brain, kidneys, and limbs), leading to ischemia, where cells of that organ may die, or the organ can deteriorate, leading to diseases like coronary artery disease, cerebrovascular disease, peripheral artery disease, chronic renal failure, etc.
Some may have a headache, dizziness, vertigo, or confusion before the stroke.
Paralysis usually lasts for more than 24 hours and can last for months, years, or a lifetime.
Some patients may experience numbness and weakness on one side of the body, a drooping mouth, slurred speech, blurred vision, or dizziness and vertigo, which usually last for about 2-30 minutes (rarely up to an hour, but never more than 24 hours) and then return to normal. This is called a transient ischemic attack (TIA).*

3. Patients with stroke due to cerebral hemorrhage often experience immediate symptoms without any prior warning signs. Some may experience these symptoms during intense physical activity or sexual activity. Patients may complain of a severe headache or a one-sided headache that is worse than any they have previously experienced, typically accompanied by nausea and vomiting. Symptoms also include a drooping mouth, inability to speak, and gradual weakening of the limbs. They may experience seizures and rapidly lose consciousness.
If the bleeding is severe, the patient often loses consciousness, has muscle stiffness, and constricted pupils in both eyes, often resulting in death within 1-2 days.
If the bleeding is not severe, there may be a chance for recovery and gradual improvement, or if surgery is done in time, it may help save the patient's life.
In cases caused by the rupture of an aneurysm or an arteriovenous malformation (AVM), typically found in individuals aged 25-50, there may be a slight blood leak before the rupture. The patient will have a continuous headache and may also have facial pain and double vision for minutes to weeks. When the vessel ruptures, there will be a sudden severe headache and loss of consciousness. The patient may remain unconscious or may lose consciousness for a while and then regain consciousness but will have confusion, drowsiness, headache, dizziness, and vomiting.

*A transient ischemic attack (TIA) occurs when there is a temporary blockage of blood flow to the brain, which may result from narrowed or clogged arteries in the brain or carotid arteries or from an embolus originating from outside the skull that lodges in a brain artery. Patients exhibit symptoms, causes, risk factors, and preventive measures similar to those of acute stroke, but the key difference is that TIA symptoms last no longer than 24 hours (most commonly just 2-30 minutes) and resolve spontaneously. The body naturally removes the blockage quickly, restoring normal blood flow to the brain.
It has been found that if a TIA is not treated, about 10-20% of patients will have a stroke within three months (about half of these strokes occur within two days after a TIA). Moreover, 15-30% of stroke patients have a history of previous TIA, making TIA a warning sign of an impending stroke. Therefore, if symptoms of cerebral ischemia occur (such as weakness on one side of the body, slurred speech, and drooping mouth), regardless of whether stroke or TIA is suspected, it is crucial to seek immediate hospital treatment. Prompt medical attention for these conditions is essential to prevent permanent hemiplegia.
- Weakness in the arms and legs, movement or walking difficulties may lead to falls, fractures, or head injuries.
- A drooping mouth, difficulty speaking, difficulty swallowing, or choking (leading to airway obstruction or pneumonia).
- Inability to perform daily activities independently, feeling like a burden to others, loss of self-confidence, withdrawal, and social isolation.
- Some may experience memory loss, slow thinking, difficulty understanding reasons, or inability to make decisions.
- Inability to control emotions, irritability, or depression.
- In cases of chronic paralysis and bedridden patients, bedsores may develop on the buttocks, back, and joints. Pneumonia or urinary tract infections are common complications that can lead to serious sepsis.
- Prolonged bed rest can also lead to deep vein thrombosis, which can cause pulmonary embolism and be fatal.
- In severe cases or those with coexisting diseases (such as heart disease and arrhythmias), death may occur from cerebral or cardiac complications.
Doctors initially diagnose based on symptoms, medical history, and a physical examination.
Physical examination, besides observing paralysis of limbs on one side, may include facial droop, speech difficulties, lethargy, high blood pressure, and hyperactive tendon reflexes. There may also be slow or irregular breathing.
In cases caused by a cerebral embolism, the physical examination might reveal heart abnormalities such as audible heart murmurs, arrhythmias, or tachycardia.
In cases of cerebral hemorrhage, patients may be less alert, unconscious, have a stiff neck, and severely high blood pressure. There may also be pupil inequality, and in severe cases, both pupils may be constricted.
In cases of a transient ischemic attack (TIA), if patients are examined after symptoms have subsided, no abnormal brain symptoms are usually found, apart from the underlying conditions or diseases causing it (such as high blood pressure, irregular heartbeat, and heart disease).
For a definitive diagnosis, doctors may perform brain imaging using magnetic resonance imaging (MRI) or computed tomography (CT). Additional diagnostic tests may include a cerebral angiogram, Carotid Doppler ultrasound, echocardiogram, lumbar puncture, blood tests, urine tests, and electrocardiogram, among others.
Doctors will admit patients to the hospital to diagnose the cause and provide treatment accordingly:
1. In cases of transient ischemic attack (TIA), where symptoms are temporary and resolve on their own, doctors will prescribe medications to control underlying risk factors such as high blood pressure, diabetes, and abnormal blood fat levels. They will also prescribe antiplatelet medications to prevent recurrent blood clots from blocking blood vessels. Aspirin 81-325 mg daily is a common choice. For patients who cannot take aspirin, clopidogrel is an alternative.
For patients with carotid artery stenosis greater than 70%, carotid endarterectomy may be necessary to remove plaque and blood clots. In some cases, balloon angioplasty and stenting may be used.
For treatment outcomes of TIA, timely and ongoing treatment not only prevents the recurrence of this condition but can also reduce the risk of subsequent stroke by up to 80%.
2. In cases of a stroke caused by cerebral ischemia due to occlusion (cerebral artery stenosis and cerebral embolism), in addition to symptomatic treatment (such as intravenous fluids, respiratory support, control of a rapid heartbeat, antipyretics for high fever, and antihypertensives for very high blood pressure), once imaging confirms the condition (and rules out cerebral hemorrhage), doctors may consider giving thrombolytic agents. This includes recombinant tissue-type plasminogen activator (rt-PA) via intravenous injection to dissolve the clot and restore blood flow to the brain, helping to prevent brain cell death and enabling a quicker recovery. This medication is most effective if given within 4.5 hours (270 minutes) of symptom onset, and patients must not have contraindications to its use (such as unconsciousness, seizures at the onset of symptoms, blood pressure > 185/110 mmHg, low platelets, anticoagulant therapy, bleeding disorders, etc.).
In some cases, doctors may prescribe anticoagulants (such as heparin) to patients with atrial fibrillation, valvular heart disease, or an increased risk of recurrent clots. If given after thrombolytic therapy (tPA), it should be given at least 24 hours apart.
Once symptoms are stable, doctors will prescribe antiplatelet medications (such as aspirin or clopidogrel) and medications to control underlying conditions or diseases. Rehabilitation will also be provided, including physical therapy and the use of assistive devices.
For patients with carotid artery stenosis, treatment may include surgery or balloon angioplasty.
Treatment outcomes depend on the severity of the condition. If the condition is mild and treated correctly from the start, the patient may fully recover or nearly regain normal function, becoming able to care for themselves, speak, and walk, though they may have some difficulty using their hands. In more severe cases or those that do not receive timely treatment, patients may experience physical disabilities or impairments that require assistance from others, such as wheelchair use or other assistive devices.
A small percentage of patients may develop severe disabilities that require bed rest and constant care or may even die while hospitalized.
Generally, physical recovery takes time. If improvement occurs, it typically begins within 2-3 weeks and continues gradually until patients can regain independence or make a near-full recovery.
3. In cases caused by a cerebral hemorrhage, treatment is symptomatic, such as intravenous fluids, intubation, mechanical ventilation, controlling blood pressure if it is severely high, etc. In cases with a significant blood clot in the brain, urgent brain surgery might be necessary. For minor bleeds that do not compress vital brain areas, surgery might not be required, and rehabilitation can proceed once it is safe to do so.
Treatment outcomes for hemorrhagic stroke depend on the location and volume of the hemorrhage, the patient's condition (age, comorbidities), and the development of complications.
Hemorrhages in the brainstem carry a high mortality rate of 90-95% and are often not amenable to treatment.
If the blood clot is large and ruptures into the brain ventricles, the mortality rate is about 50%.
If the bleeding is on the brain surface or involves a small blood clot that does not rupture into the ventricles, the mortality rate is lower.
Patients with severe symptoms who survive often suffer from permanent disabilities. Some may end up in a vegetative state for many years and eventually die from complications such as pneumonia or various infections.
Younger patients who experience hemorrhages due to congenital vascular abnormalities may make a full recovery if the rupture occurs in a non-critical location and they receive prompt and appropriate treatment.
Some post-surgical patients, even if they recover physically well, may develop post-stroke epilepsy, requiring lifelong anticonvulsant medication.
Once diagnosed with acute stroke or transient ischemic attack (TIA), follow the doctor’s instructions for treatment and care.
Once treated and able to recover at home, self-care should include:
- Follow your doctor's instructions carefully for taking medication and follow-up appointments.
- Eat a healthy diet (reduce sweet, fatty, and salty foods), lose weight (if overweight), get enough sleep, find ways to relax (such as chanting, praying, or meditating), and exercise (as much as your body allows).
- Do not smoke or drink alcohol.
- Avoid buying and using medications, herbs, or supplements on your own. If you want to use them, consult your doctor about their benefits and safety, as they may have side effects that can lead to liver or kidney damage or interact with medications you are taking (enhancing or counteracting the effects of the medications), resulting in poor disease control or harmful side effects (such as bleeding or low blood sugar).
- Continue with physical therapy as instructed by your doctor/physical therapist. This may include exercises such as frequently stretching and bending all joints of the arms and legs to prevent stiffness, regularly exercising muscles, and trying to use the arms and legs to promote faster recovery (if the patient is inactive and does not try to use the arms and legs, the muscles will atrophy and stiffen). Practice walking, speaking, and writing.
- For bedridden patients, use a pressure-reducing mattress (such as a water or air mattress), and caregivers should turn the patient every 2 hours to prevent bedsores on the buttocks, back, and joints.
- Provide adequate food and water. Some patients may need tube feeding (through the nose or abdomen into the stomach). If dehydrated, the patient may become lethargic, or their condition may worsen. Be careful when feeding the patient; do not let them choke.
- If there is a urinary catheter or feeding tube, keep it clean and safe, and change it as instructed by your doctor/nurse.
- High fever, chills, diarrhea, vomiting, cloudy or bloody urine.
- Severe headache, confusion, drowsiness, reduced consciousness, seizures, or difficulty breathing.
- Difficulty eating or drinking.
- Development of pressure sores.
- Medication is lost, there is a shortage of medication, or you suspect side effects or allergic reactions to medication, such as hives, itchy rash, blisters, swollen eyes, swollen mouth, nausea, or vomiting.
- Increased anxiety.
- Quit smoking and avoid heavy alcohol consumption. Reduce salt and sugar intake, cut down on foods high in fat, and lose weight if overweight. Regular physical exercise is also recommended to prevent premature arteriosclerosis.
- Regularly check for high blood pressure, diabetes, and cholesterol levels. If abnormalities are found, they should be treated seriously and consistently. Controlling these conditions can reduce the risk of stroke.
- If you suffer from sleep apnea, seek treatment and manage any associated risk factors and complications (such as obesity, high blood pressure, diabetes) to lower the risk of stroke.
- If you experience temporary weakness of the limbs due to a transient ischemic attack (TIA), consult a doctor promptly. Follow medical advice and take prescribed medications regularly to prevent a stroke caused by blood clots in the brain.
- Patients with heart conditions, such as rheumatic heart disease, those with artificial heart valves, arrhythmias, or myocardial infarction, should manage their condition and consistently take aspirin or other antiplatelet drugs as prescribed to prevent blood clots in the heart that could travel to the brain and cause a stroke.
1. Transient ischemic attack (TIA) is characterized by short-term symptoms that disappear either at home or during the trip to the hospital. This can lead patients and their families to underestimate the seriousness of the condition and neglect seeking medical treatment. Patients who experience TIA are at a high risk of recurring symptoms or progressing to a stroke later on. Therefore, if symptoms of a cerebral vascular event occur, it is crucial to visit a hospital promptly to receive safe treatment and prevent potential disability.
2. This disease is often chronic. Recovery from a stroke can vary; some patients may recover quickly and become independent, while others may recover slowly or suffer from permanent disabilities. However, the cognitive functions of most patients remain intact. Relatives should show empathy, engage in conversations, and encourage participation in activities (such as reading, writing, hobbies, and social outings) as much as the patient's physical condition allows to stimulate their brain and enhance their sense of self-worth.
3. For those who have recovered well or have minor weakness but can move around effectively, they are able to work and live normally, though they may still need to travel with assistance. Nonetheless, patients must continue to manage their health, attend regular medical follow-ups, and remain vigilant for any signs that may indicate a relapse.