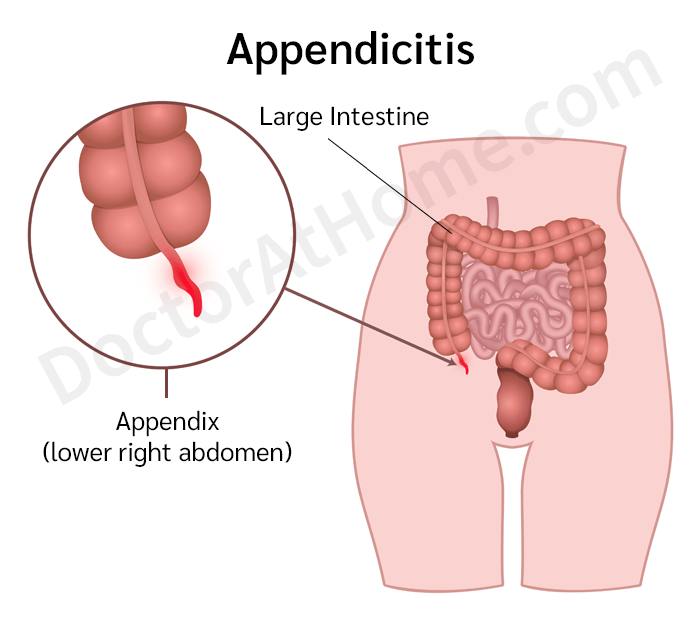
Appendicitis is the most common cause of severe abdominal pain requiring surgery. If lower right quadrant pain is present, this condition should always be considered first. It is a common disease in people of all ages, most frequently found between 10 and 30. Appendicitis is less common in children under three (due to a wider appendix base) and in elderly individuals (due to less remaining appendix tissue). There is a slightly higher prevalence in males than females, with an estimated lifetime risk of 7% and an incidence of 1 in 1,000 people per year.
The primary cause of appendicitis is a blockage of the appendix*, most often by hardened stool particles known as fecaliths. Other potential causes include foreign objects (e.g., fruit seeds), enlarged lymphoid tissue within the appendix, parasites (especially roundworms), and tumors. The blockage prevents normal appendix drainage, leading to fluid congestion, swelling, and increased pressure. This pressure, combined with the appendix's contractions to expel the item, causes pain near the navel. Meanwhile, bacteria within the appendix will multiply rapidly, infecting the appendix tissue and leading to severe inflammation. Patients will experience pain in the lower right abdomen, and ultimately, the appendix tissue may become necrotic and rupture.
In some cases, particularly in AIDS patients, cytomegalovirus (CMV) infection can trigger appendicitis.
Occasionally, the cause of appendicitis is unknown.
*The vermiform appendix is a 3-4-inch-long tube extending from the cecum (the uppermost part of the large intestine) situated in the lower right abdomen. It is considered a part of the large intestine that has atrophied and no longer functions in food digestion and absorption. Due to its being a small, blind-ended tube, inflammation can rapidly lead to necrosis and rupture (perforation).
The key feature of appendicitis is continuous, progressively worsening abdominal pain lasting over 6 hours. If left untreated, the pain can persist for days, eventually becoming intolerable and necessitating hospitalization.
The condition often begins with sensations of fullness in the upper abdomen, similar to gastritis or cramping pain around the navel, resembling diarrhea symptoms. Patients might feel a frequent urge to defecate, though no stool is passed (some may resort to using enemas or laxatives). In some instances, watery or loose stools may also occur.
A common accompanying symptom is a loss of appetite. The absence of this symptom may indicate alternative diagnoses.
Following the onset of abdominal pain, patients frequently experience vomiting (nausea might precede the pain), typically only 1-2 times. If vomiting occurs before any abdominal pain, appendicitis is less likely.
The abdominal pain is often persistent and cannot be relieved by pain medications.
Within 4-6 hours, the pain will shift to the lower right abdomen, becoming steady and intensifying upon movement, walking, coughing, or sneezing. Patients are often forced to minimize movement, adopt a fetal position, or walk stooped over for relief.
Fever or mild feverish symptoms are also possible.
Approximately half of those with appendicitis patients may not exhibit these typical symptoms; they might experience right lower abdominal pain without any preliminary signs.
Children's symptoms may not be as clear or distinct as in adults. For example, they may have generalized abdominal pain (not limited to the lower right abdomen) or fever with less obvious abdominal tenderness.
In the elderly and pregnant women, abdominal pain may not be severe, and symptoms may be less pronounced, leading to delayed diagnosis and increased risk of complications.
If left untreated, the appendix may become necrotic and rupture, spreading infection throughout the abdominal cavity. This results in peritonitis (inflammation of the stomach lining) and sepsis, both of which are life-threatening conditions. Additionally, an abscess may form around the ruptured appendix. These complications typically develop within 24-36 hours following the onset of inflammation.
Complications are more common in young children, the elderly, and diabetic patients. The mortality rate in elderly patients with appendicitis is as high as 15%.
Doctors will diagnose appendicitis based on clinical symptoms and examination findings:
A slight fever (37.5-38 degrees Celsius, usually not exceeding 38.5 degrees Celsius). However, not all patients exhibit fever.
Tenderness in the lower right abdomen, particularly at the appendix or McBurney's point, is a key diagnostic indicator.
If this area is gently pressed and quickly released, the patient will feel strong pain upon the rebound. This is called rebound tenderness, suggesting the onset of peritoneal inflammation in the area.
The patient may also feel pain in the lower right abdomen when pressing on the lower left abdomen (called Rovsing's sign).
If the appendix has ruptured, the patient may exhibit generalized abdominal pain and a rigid abdomen. A mass may be palpable during an examination, and the patient might have a high fever.
The physician, wearing gloves, will perform a rectal examination by inserting an index finger into the patient's rectum. If touching the appendix elicits significant pain, the finding will support the diagnosis of appendicitis.
In cases where further confirmation is necessary or to distinguish appendicitis from other conditions, additional tests may be employed. These include blood tests (often show an elevated white blood cell count in appendicitis patients), urine tests (if the appendix is close to the ureter or bladder, there may be abnormally high red and white blood cell count), computed tomography (CT) scans, or ultrasound (may show swollen, inflamed appendix or an abscess in the surrounding area).
If appendicitis is suspected, the patient will be hospitalized and treated with urgent appendix removal surgery. Antibiotics are administered by injection prior to surgery to prevent postoperative infections. Typically, patients without complications may stay in the hospital for 2-5 days and usually recover without further issues.
In cases where complications arise, such as a ruptured appendix, the treatment becomes more challenging, and the patient's hospital stay may extend for weeks.
If you have symptoms that are indicative of appendicitis, such as severe, continuous abdominal pain lasting more than 6 hours or pain that worsens when the abdomen is pressed or jolted, especially in the lower right abdomen, you should consult a doctor promptly.
Once diagnosed with this condition, you should follow the doctor's advice and treatment plan and attend follow-up appointments.
For those given medication, if you experience any side effects (such as allergic reactions, rashes, blisters, swelling of the eyes and mouth, nausea, vomiting, or other unusual symptoms), see a doctor before the scheduled follow-up appointment.
Currently, there are no effective methods to prevent appendicitis.
Ideally, when symptoms indicative of appendicitis occur, see a doctor directly. Early treatment can lead to faster recovery and minimize the risk of complications.
1. Appendicitis is a serious condition that requires immediate surgical intervention. Medications, whether oral or injectable, provide only temporary symptom relief. Delaying treatment until the appendix ruptures can lead to complications such as wound infections, increased medical costs, longer hospital stays, and higher risks of death (a mortality rate of 3% for complicated cases compared to less than 0.1% for uncomplicated cases).
2. Right lower abdominal pain can stem from various causes other than appendicitis, including ureteric stones, salpingitis, menstrual pain, and ectopic pregnancy, each with distinct symptoms.
However, persistent abdominal pain lasting over 6 hours, or pain worsening when moving or pressing in the lower right abdomen, whether presented with fever or not, should be suspected of appendicitis or other serious conditions. Patients should immediately seek the nearest medical care. Do not dismiss the pain as routine or regular abdominal discomfort, such as menstrual pain.
3. Patients with appendicitis may not exhibit classic symptoms, with over half of the patients not reporting initial pain around the navel. Some may have abdominal pain along with constipation or diarrhea. The pain may not always localize to the lower right abdomen if the appendix is abnormally positioned.
If you experience frequent abdominal cramping without defecating, avoid assuming it is merely constipation, and avoid using enemas or laxatives, as it may cause the appendix to rupture.
Early symptoms of appendicitis can resemble gastritis, with pain starting under the upper abdomen or around the navel. Therefore, close monitoring of these symptoms is crucial. If pain persists despite taking gastritis medications, worsens, or shifts to the lower right abdomen, consider appendicitis, particularly if the pain persists for over 6 hours.
4. Patients with appendicitis may present with a slight fever or none. A high fever might indicate a ruptured appendix or other conditions such as typhoid, salpingitis, or acute pyelonephritis.
5. A simple initial check for appendicitis is gently pressing the lower right abdomen with a finger. If there is significant pain in that area, suspect appendicitis. This check should be considered for anyone presenting with abdominal pain or diarrhea.